Meet Ms. Ferro, a 29-year-old from Vienna.
Despite childhood tonsil and adenoid removal, cosmetic rhinoplasty, and persistent attempts to improve her breathing, she continued to struggle with nasal obstruction, fatigue, and mouth breathing—even during yoga practice.
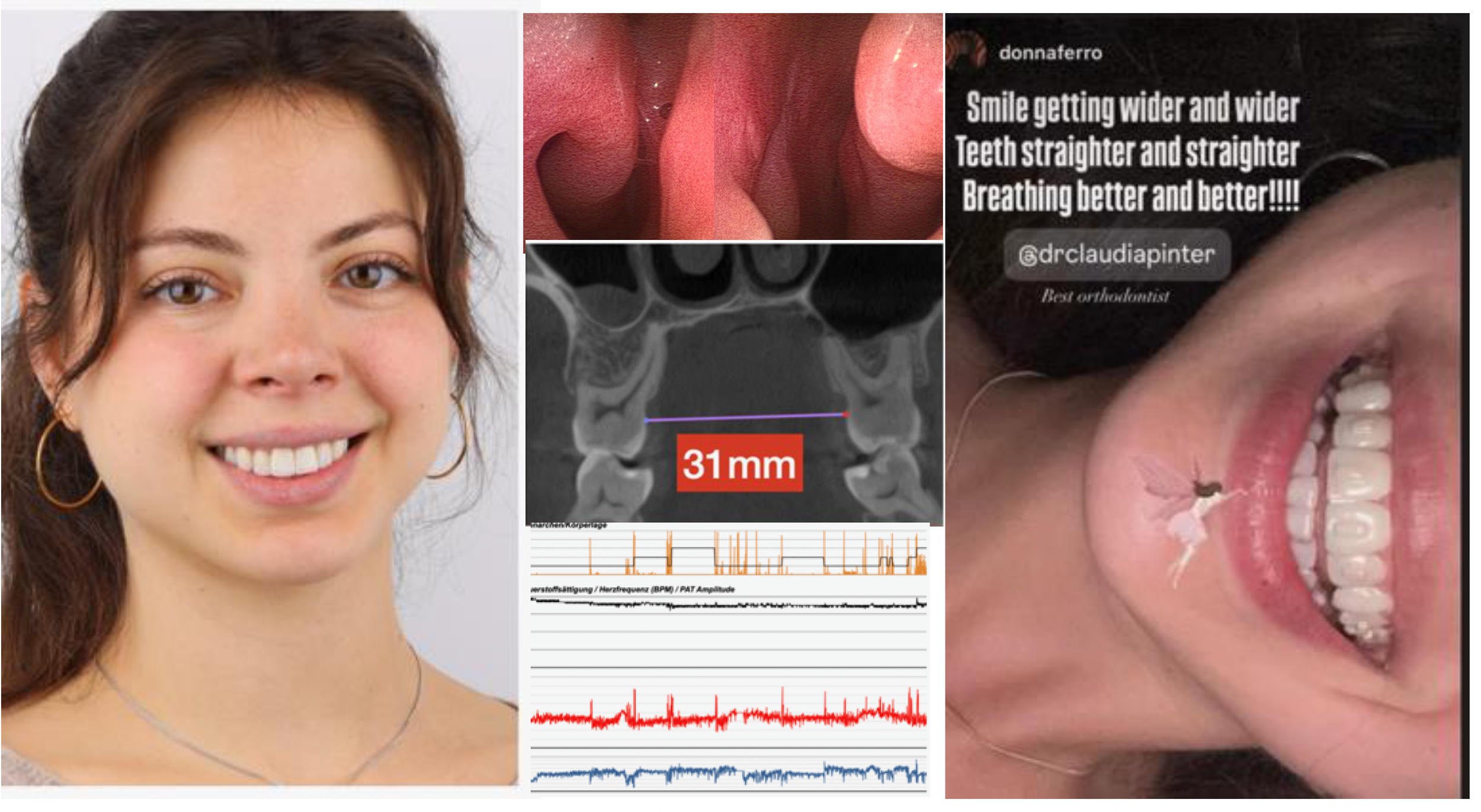
In Dr. Claudia Pinter’s office, she presented with a “perfect bite” (Class I occlusion). Yet her upper first molar-to-molar width measured 31 mm—well below the ideal 36–38 mm. Could transverse maxillary hypoplasia explain her lifelong breathing difficulties? And does it justify maxillary expansion when her “bite” is “fine”?
While visiting Miami, Ms. Ferro sought consultation with Dr. Stanley Liu, an experienced sleep surgeon. Her home sleep study from Vienna looked “normal,” but her symptoms told a different story. Careful history, nasopharyngoscopy, and exam revealed a mucosal band tethering the septum to the inferior turbinate, a small septal perforation, and transverse maxillary hypoplasia. Moreover, shortcomings in the home sleep study were identified. Taken together with her fatigue, these findings suggested Upper Airway Resistance Syndrome (UARS) - a condition often missed in a seemingly “healthy” population.
For patients like Ms. Ferro, nasal surgery may fall short. She underwent DOME (Distraction Osteogenesis Maxillary Expansion) with Dr. Pinter in Vienna, using the non-diastema protocol—a technique that expands the maxilla and nasal floor without creating a midline gap, preserving aesthetics while restoring function.
Cases like this underscore why orthodontics and sleep medicine must work together to evaluate subtle skeletal phenotypes, recognize when at-home sleep studies fall short, and deliver treatments that transform lives.
This is exactly what we teach in the DOME Course: how to identify complex airway patients and apply advanced expansion protocol to achieve lasting results in sleep-disordered breathing.